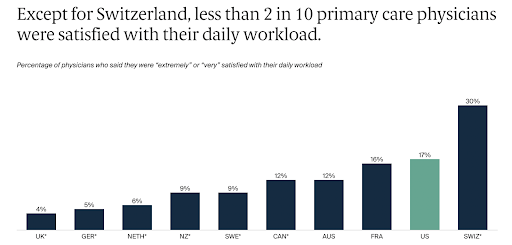
The 2022 International Health Policy Survey’s findings reveal a striking trend among primary care physicians globally, with the exception of Switzerland, where less than 20% express satisfaction with their daily workload. This statistic is indicative of a widespread issue in the healthcare sector, where physicians are increasingly facing excessive workloads that are unsustainable in the long term. Factors contributing to this dissatisfaction include long working hours, high patient volumes, and the complexity of cases they handle. Additionally, the administrative burdens associated with modern medical practice, such as paperwork and electronic health record management, consume a significant portion of their time, further exacerbating the problem. The situation in Switzerland, which stands as an outlier, suggests that there are systemic approaches or practices in place that better manage physician workloads, offering insights that could be beneficial for other healthcare systems globally. The overall trend highlighted by the survey underscores the need for healthcare systems worldwide to reevaluate and restructure how primary care is delivered, ensuring that physicians can manage their workloads effectively while maintaining high standards of patient care.
Sarah M. Worthy, CEO of DoorSpace explains why so few physicians are satisfied with their daily workload. “Less than 20% of primary care physicians reported satisfaction with their daily workload – which is not surprising when you start to look at how much non-patient related work we demand from them. Primary care physicians are spending the majority of their time on tasks such as phone calls with insurance companies, filling out patient charts, and keeping track of the myriad of credentials, training, and professional licensure they’re required to maintain.”
Financial incentives often lead physicians to prioritize certain treatments or procedures, potentially influencing medical decision-making. This can create ethical dilemmas where the best interest of the patient may not always align with the financially beneficial choices. Consequently, this dynamic can further contribute to physician dissatisfaction and moral distress, as they navigate the complex interplay between healthcare delivery and economic imperatives.
“At the center of this issue is a focus by healthcare leaders on the financial side of healthcare at the expense of both patient quality care as well as clinician satisfaction. Healthcare leaders must put people before profits. If they’re unable to do this, then patients and clinicians have to work together to demand laws are put in place that protect the human side of healthcare,” Worthy shares.
Healthcare leaders must prioritize the well-being of their staff, recognizing that the quality of patient care is directly linked to the satisfaction and support of their physicians. It’s imperative that healthcare organizations begin to genuinely value their physicians not just as revenue generators, but as vital contributors to the overall health and well-being of society. This shift in perspective involves investing in better working conditions, offering competitive compensation, and providing adequate mental health support. Additionally, organizations should foster an environment where physicians feel heard and respected, ensuring their opinions and expertise are integral in shaping policies and practices. By genuinely valuing their physicians, healthcare organizations can create a more sustainable and effective healthcare system.
The findings from the 2022 International Health Policy Survey paint a concerning picture of the current state of primary care across the globe, with physician dissatisfaction stemming from unsustainable workloads and the impact of financial incentives on medical decision-making. The need for systemic changes in healthcare is evident. Healthcare leaders and organizations must shift their focus from profit-driven models to ones that prioritize the well-being of physicians and patients alike. This includes creating supportive work environments, aligning financial incentives with patient care, and involving physicians in policy decisions. By addressing these issues, the healthcare sector can improve physician satisfaction, which is crucial for maintaining high standards of patient care and ultimately ensuring the sustainability of healthcare systems worldwide.